Personalization in Pediatric Value-Based Care: A Path to More Safe Days at Home
Jan 5, 2026
Executive Summary
Many children with special health care needs and their families live with constant uncertainty, navigating a healthcare system that was designed to be reactive to acute crises rather than proactive in continuous and ongoing support. Pediatric value-based care offers a transformative path forward and seeks to improve long-term outcomes, yet its full promise will only be realized for this population if care models reflect the unique, evolving, and longitudinal needs and the central role of family experiences and caregiver voices.
Children with special health care needs and their caregivers experience far greater challenges accessing care than most families. They require more personalized, flexible care that adapts to their changing circumstances. The Imagine Pediatrics team-based virtual and in-home model is purpose-built for these children. Through specialized programming and an integrated pediatric care model, multidisciplinary teams deliver both acute and longitudinal care 24/7 — addressing medical, behavioral, and social needs holistically and changing the trajectory of each child’s health journey. For these families, success isn’t measured only by fewer preventable hospitalizations. It’s measured more deeply in safe days at home — days when the child is engaged, stable and supported, and caregivers feel confident managing care. Imagine Pediatrics partners with families, health plans, providers, and community resources to make that stability possible.
This white paper explores where the current healthcare system falls short, what truly personalized pediatric care looks like, and how the Imagine Pediatrics unique care model offers a better way forward. It’s both a snapshot of what’s working and a call to reimagine pediatric health care. Together.
A Story from Claire and Koa

Claire Kouns is mother and caregiver to Koa, a four-year-old boy and an Imagine Pediatrics patient with congenital diaphragmatic hernia and cerebral palsy among other concurrent conditions. Claire says that Imagine Pediatrics has made a life-changing impact on their lives and they’ve had more time at home together than ever before. She feels more in control of his care, both in times of calm and in times of crisis.
She shares an example, “On Memorial Day, Koa developed a fever and respiratory issues. Every clinic was closed and I was worried we would end up in the emergency room. I called Imagine Pediatrics and spoke with our pediatrician, and they sent out the Mobile Integrated Care team to check on Koa. The team came to our home, ran swabs, and quickly identified the infection. Before leaving, they administered his first round of antibiotics and made sure Koa had what he needed that same day. Thanks to Imagine Pediatrics, my child with complex medical needs was able to stay at home rather than going to a crowded ER surrounded by even more illness. It truly was a lifesaver.”
The Problem: Pediatric Care Isn’t Built for Families with Complex Medical & Behavioral Health Needs
One in five U.S. children, nearly 14.5 million, has a special health care need. This population accounts for half of all pediatric health spending, yet too often the system fails to provide the coordinated, continuous care they require. These children are frequently misunderstood to be a small group with rare conditions, when, in fact, they represent a highly diverse population with diagnoses across more than 40 medical and behavioral therapeutic areas, many that are co-morbid. They need personalized, holistic, consistent support that adapts as they grow — but most experience fragmented and reactive care instead.
Across all coverage types, families report major challenges with access. Only 78 percent of children with special health care needs have a consistent healthcare provider, and nearly one in five cannot access the mental health treatment they need. More than one in five families say they need extra help coordinating care, yet many never receive it. These gaps leave families managing complex conditions with limited support, often leading to preventable crises and hospitalizations.
For children covered by Medicaid, barriers are even greater. These families report difficulty getting appointments, and 37 percent report at least one emergency department visit in the past year — nearly twice the rate of privately insured children. Although Medicaid offers comprehensive coverage, differences in coordination, access, and continuity across geographies continue to drive challenges with fragmentation of care.
Without an approach that connects medical, behavioral, and social support, caregivers shoulder the responsibility of navigating fragmented networks, adding emotional and financial strain. The result is a system built to react to emergencies rather than prevent them — one that leaves families on the edge of crisis instead of placing them at the center of care.
Children with special health care needs deserve better. They require data-driven, proactive, and fully integrated care that evolves with them. They need coordinated medical, behavioral, and social support that extends beyond 15-minute appointments. Yet more than one-third of families still report barriers to these integrated services, a gap that keeps too many children and caregivers in a cycle of instability.
The shift toward pediatric value-based care offers an opportunity for change. This approach provides aligned opportunities between health plans, providers and children with special health care needs so providers can spend the time needed to understand family circumstances, coordinating across systems, and following up on medical, behavioral, and social needs. It aligns incentives and outcomes for providers, health plans, and families around prevention, stability, and continuity. In today’s healthcare environment, any model that aims to be innovative and scalable must rest on a foundation of value-based care that reflects the realities of children with special health care needs and their families.
Personalization: The Missing Ingredient
Across healthcare, “personalization” is often used as a catchphrase. In pediatric value-based care, especially for children with special medical, behavioral, and social needs, it is the foundation of effective care.
Personalization means tailoring every aspect of care for the child and family. It requires attention to medical conditions, developmental stage, mental health, home environment, caregiver capacity, access to resources, and cultural context. Children with special health care needs often face challenges that extend far beyond medical diagnoses. A child’s health may be affected by food insecurity, housing instability, transportation barriers, or a caregiver’s own health and capacity to care for their child in a fragmented, low-resourced system. Personalized care addresses all of these variables and incorporates specialized services such as nutrition, palliative care, and pharmacy, all coordinated into an integrated care plan co-created with the family. Personalized care reinforces and supports the existing care plans from the child’s medical home PCP and specialists. Every child presents a unique constellation of needs, and every family brings its own strengths and challenges that call for a personalized response.
For example, two children with the same diagnosis may require very different approaches depending on how their condition presents, how they respond to medication, and the resources available in their family setting. Personalization in pediatrics therefore demands genuine insight into the child’s daily life. That insight is drawn from multiple sources, including clinical data across electronic health records and information exchanges, and most importantly, the caregiver’s knowledge and priorities.
Caregivers must be active partners in shaping care plans. Research demonstrates that when caregivers are empowered, engaged, educated, and supported, children achieve better outcomes and costs decline. Family-centered approaches are linked to stronger self-management and adherence to treatment plans, better care coordination, and fewer preventable hospitalizations. In practice, this means the most effective personalized care plans are those co-created with caregivers who are supported, reflecting not only the unique needs of the child but also the lived experience of the family.
For caregivers, support often extends to shared decision-making — having a trusted partner who can help weigh options, align care choices with family values, and provide guidance when decisions feel overwhelming. Personalization is more than customization. It’s about building trust and adapting care delivery to real-life circumstances. Families often say what matters most is feeling heard, respected, and supported as well as knowing that someone familiar with their child will be there when they call, 24/7.
From Personalization to Continuity
Personalization leading to continuity means care that is cohesive, proactive, and steady over time, built in collaboration with health plans, the patient’s medical home primary care providers, and specialists. When families work longitudinally with an empaneled team that knows their history, understands their goals, and stays involved through every stage, the result is stronger relationships, earlier interventions, and better outcomes.
Continuity is vital in pediatrics, where children’s health can shift quickly as they grow, and where transitions – from hospital to home, from one specialist to another, or from crisis back to stability – are frequent. Often, immediate care from the patient’s medical home primary care provider is not available 24/7, and when round-the-clock care can be provided in a way that collaborates with the PCP’s care plan and meets the patient and family’s immediate need, outcomes improve. Personalized care also makes these transitions smoother and relieves the stress families often face when trying to navigate the system on their own.
A strong pediatric value-based care model makes continuity possible by assigning each child and family a consistent, multidisciplinary team that stays engaged across time and settings. Consider a child diagnosed with ADHD who begins to struggle with focus, peer interactions, and frustration at school. Because the care team already knows the child and family, they can recognize subtle behavioral changes and act before problems escalate. The physician reviews medications, the behavioral health clinician works with the caregiver and teachers to reinforce coping and social skills, and the care coordinator checks in regularly to monitor progress and can collaborate with the school and other providers. By collaborating across medical, behavioral, and social supports — and by keeping the caregiver involved in every decision — the team helps prevent academic and emotional decline, reduces stress at home, and keeps care steady over time.
What could have been a traumatic, episodic encounter instead becomes a coordinated process that stabilizes the child in the moment and sustains progress over time. This is what continuity looks like in practice: a care experience that feels less like a series of transactions and more like a true partnership built on trust that delivers better outcomes.
Technology as an Enabler of Personalization and Continuity
Technology in pediatric care is not a standalone solution. It is the infrastructure that supports continuous, family-centered care — keeping the focus on children and caregivers while technology works to support the care. When designed around the needs of families and clinicians, it reduces fragmentation, simplifies communication, and turns data into actionable insights that guide next steps.
The Imagine Pediatrics clinical model is powered by a technology ecosystem that connects the care team, the family, and data in real time. This ecosystem, anchored by our proprietary Care Hub platform and seamlessly integrated with our family-facing mobile app, keeps care coordinated and responsive 24/7. The result is a technology foundation that enables true collaboration and communication, closes gaps, and delivers better outcomes and experience.
Next-Generation Population Health Management: Care Hub as the Central Nervous System
Care Hub is more than a population health management (PHM) platform. It is the digital central nervous system of our care delivery model, purpose-built for pediatric and family-based care. Unlike traditional PHM tools that operate in silos, Care Hub unifies medical, behavioral, and social data across multiple sources and stakeholders into a single, dynamic environment for our care teams.
By combining electronic health record (EHR) data, claims, social determinants, behavioral health, and patient-reported information, Care Hub generates a comprehensive, 360-degree view of every child and family. Advanced analytics within Care Hub help us understand the heterogeneity of each patient and surface changes and opportunities early. We’re able to quickly identify gaps in care and recommend personalized next best actions to the care team, transforming raw data into actionable insights for proactive outreach instead of waiting for a crisis. Care Hub enables secure, bi-directional data sharing with external providers, health systems, and community organizations, promoting true care coordination across the ecosystem.
With Care Hub, we can manage care for families, not just individual patients. It incorporates the complex consents and permissions unique to pediatric and foster care settings, ensuring that caregivers, clinicians, and authorized stakeholders all have appropriate visibility and access.
Family Access and Experience
Like Care Hub, The Imagine Pediatrics caregiver and patient-facing mobile app also enables connection. With the app, caregivers connect directly with the care team 24/7, enabling both longitudinal and acute care through telehealth, messaging, and home-based support. Because the app is fully integrated with Care Hub, the family’s digital experience is tightly linked with the clinical workflow, ensuring that every interaction, update, and care plan adjustment is reflected seamlessly across the system. The Imagine Pediatrics mobile app features a family-focused design that supports multiple children and care settings, delivering personalized care plans, educational materials, and consistent access to familiar team members who already know each child’s history, reinforcing continuity and trust. Caregivers can seamlessly transition from chat to video visits within seconds.
Our app is purpose-built for families of children with special health care needs and the technology adapts to barriers such as unreliable internet, language differences, and caregiver schedules, offering multiple engagement options including app-based chat, multi-tenant video, phone calls, or in-home visits.
And for rural or underserved families, mobile connectivity combined with in-home support reduces disruptive travel to distant emergency departments, hospitals, or specialists. The bi-directional data input through the app ensures that care teams are continuously informed, enabling context-aware, proactive care and preventing caregivers from repeating their child’s story.
This technology infrastructure makes scalable personalization possible. It connects families, care teams, and partners in real time, ensuring continuity across medical, behavioral, and social needs. For children with special health care needs, it means earlier interventions, fewer preventable hospitalizations, and more safe days at home. And for pediatric value-based care, it demonstrates how technology can translate data and integration into measurable improvements in outcomes, experience, and cost — fulfilling the true promise of value-based care.
Common Pitfalls in Today’s Pediatric Value-Based Care
Despite growing adoption of value-based-care (VBC) across the healthcare landscape, many pediatric VBC programs fall short, especially for children with special health care needs. Here are some of the most common pitfalls:
- Models not built for pediatrics. Most existing value-based care models were designed for adults with a largely homogeneous set of conditions, like diabetes, heart disease, and cancer. And, because these diseases are common with age, diagnosis and treatments are well established. However, children with special health care needs face rare or heterogeneous conditions with evolving trajectories. Because of this heterogeneity and the constantly changing developmental, medical, behavioral, and social demands these children require integrated, responsive care. Pediatric value-based care must deliver that care where and when families need it, so children can stay healthy and have more safe days at home.
- Rotating care teams with little continuity. Children with special health care needs require providers who know their history and context. Often, families must re-explain their story at every touchpoint, risking details being lost and taking valuable time away from deeper conversations around care plans or a crisis moment at hand.
- Technology without interoperability. Good data can drive action, but only if data streams are standardized and interoperable. When data is fragmented, so is the care. And when care is fragmented, poorer outcomes are the result.
- Inflexible payment models. Many current alternative payment models (APM) lack the flexibility to support the dynamic, long-term nature of pediatric care. They often fail to account for multidisciplinary coordination, family engagement, and the ongoing adjustments required as children grow and their needs change. Current APMs incentivize for face-to-face, appointment-driven care, yet the care required for these children often happens outside of a traditional in-office scheduled appointment. Today’s pediatric patients, especially adolescents, and their caregivers are digitally savvy and want new modalities to engage when they need care, where it is most accessible to them. Yet most APM frameworks are built from the foundation of a fee-for-service claims-based chassis that doesn’t adapt and allow for the new and innovative modalities of providing care.
- Failure to elevate the caregiver voice. Families bring essential context and are typically health knowledgeable and know what their children need. Yet too often they are treated as coordinators rather than collaborators and are not given the opportunity to transform their knowledge into clinical care. Excluding their perspective makes it difficult to build trust and to implement care plans successfully.
These shortcomings can erode trust, increase burnout, and keep families, providers, and health plans locked in a reactive, crisis-driven system. The result is frustration for caregivers, administrative burden for clinicians, and unsustainable costs for health plans. A better approach centers on personalization, team continuity, integrated longitudinal care, and true family partnership from the start.
Policy and Payment Considerations
To further expand on the pitfall of inflexible payment models, government policy and care delivery are deeply interconnected, especially for vulnerable populations like children with special health care needs. Yet most policies still overlook that the family is central to a child’s health. When policymakers and plans invest in families — ensuring caregivers have the tools, training, and stability they need — the return is measurable in better outcomes, improved access, and lower costs.
Achieving this requires a shift in how we define “value” in value-based care. For pediatric populations, value cannot be measured solely by utilization or cost. It must include family-centered success metrics such as continuity, trust, and safe days at home. Progress depends on policies and payment models that expand access, strengthen collaboration between caregivers and care teams, and enable systems that measure what truly matters: the well-being and stability of children and families.
To help pediatric value-based care deliver on its promise for children with special health care needs, policies should:
- Develop pediatric-focused alternative payment models that replace crisis-driven care with proactive, integrated approaches across medical, behavioral, and social needs.
- Promote consistency in regulations to reduce churn and encourage long-term investment in value-based innovation.
- Strengthen state funding for pediatric value-based care to ensure sustainability and equitable access for children with complex needs.
- Advance data interoperability so providers, health plans, and families can share real-time information and accountability for outcomes.
- Incorporate pediatric-specific quality measures that capture trust, stability, and longitudinal progress, not just cost containment.
The Model That Makes It Possible
At the core of the Imagine Pediatrics model is a dedicated, multidisciplinary care team that includes a pediatrician, nurse, behavioral health specialist, pharmacist, dietitian, social worker, care navigator, and others. Patients are empaneled to this team throughout their care journey, creating trust and consistency for both patients and families.
Teams don’t just respond to illness but work longitudinally with families to anticipate and address the wide-ranging needs that shape a child’s health and a family’s ability to manage their overall wellness. For example, one team might help a nonverbal child with a rare genetic disorder manage feeding challenges and medications while also assisting the caregiver with school coordination and community resources.
By connecting the dots across medical, behavioral, and social needs, the care team functions like a trusted extension of the family and existing care teams as part of a medical home. And because this care is delivered both virtually and in-home, families get timely support without the strain of travel, long waits, or conflicting schedules.
The integrated virtual and in-home pediatric care model is informed by deeply listening to and understanding our patient and caregiver concerns and needs. The Imagine Pediatrics Patient and Family Advisory Council is made up of caregivers of children with special needs who advise us on our care model and how we deliver care, enabling us to truly understand how the model impacts the lived experience of our families.
Safe Days at Home: A New Benchmark for Success in Value-Based Pediatric Care Outcomes
For families of children with special health care needs, the most meaningful outcome is a “safe day at home” — a day when the child is clinically stable, when the caregiver feels confident and supported, and when the risk of crisis is low.
Safe days at home is a guiding benchmark of success for Imagine Pediatrics. When it comes to children’s health, success is often measured by what can be prevented – emergency visits, hospitalizations, and crises. Instead of managing children at the edge of crisis, we should be enabling safe, stable, and supported days at home where families feel confident, not fearful. Imagine Pediatrics believes in this work because families deserve better care, and outcomes show that Imagine Pediatrics is uniquely positioned to deliver it. Traditional metrics reward volume, not overall well-being. More safe days at home centers around the family’s lived experience. It reflects quality, continuity, and trust in care.
To get safe days at home adopted as a broader measure in pediatric care requires a collaboration of all the stakeholders in the healthcare ecosystem. Plans, providers, and policymakers must embrace family-centered success metrics and commit themselves to support pediatric access, stability, and better outcomes. This requires rethinking what we define as “value” in value-based care and a deeper understanding of how expanding access to care and close collaboration with a child’s caregiver and existing care team can improve both outcomes and experience. It demands collaboration across systems to measure what truly matters.
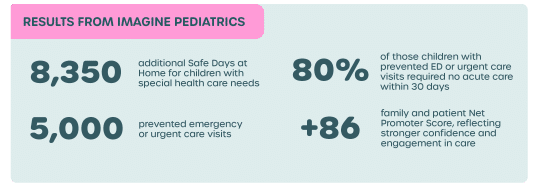
This outcome is simple, powerful, and measurable. Imagine Pediatrics helped deliver more than 8,350 safe days at home for children with special health care needs over an 18-month period. It reflects the goals of both families and value-based care arrangements. It shows that this integrated care model is working – not just for the child and their family, but for the greater good of our healthcare system.
Patient Case Study: The Impact of Safe Days at Home
An Imagine Pediatrics team began caring for a patient with multiple concurrent conditions including Lennox-Gestaut syndrome, epilepsy, and autism.
CHALLENGES & SOLUTIONS
| The Challenge | The Solution |
| Seizures and behavioral health needs cause challenges with school | Caregiver expressed concerns around missed school days due to behavioral health needs |
| Needs related to DME, nutrition, pharmacy & specialists were overwhelming the family | Imagine Pediatrics obtained a wheelchair for the patient and coordinated with the PCP to adjust formula through dietician support and pain management through palliative care |
| Caregiver expressed concerns around missed school days due to behavioral health needs | Imagine Pediatrics provided crisis intervention and assisted with school communication around enrollment and truancy laws for children with disabilities |
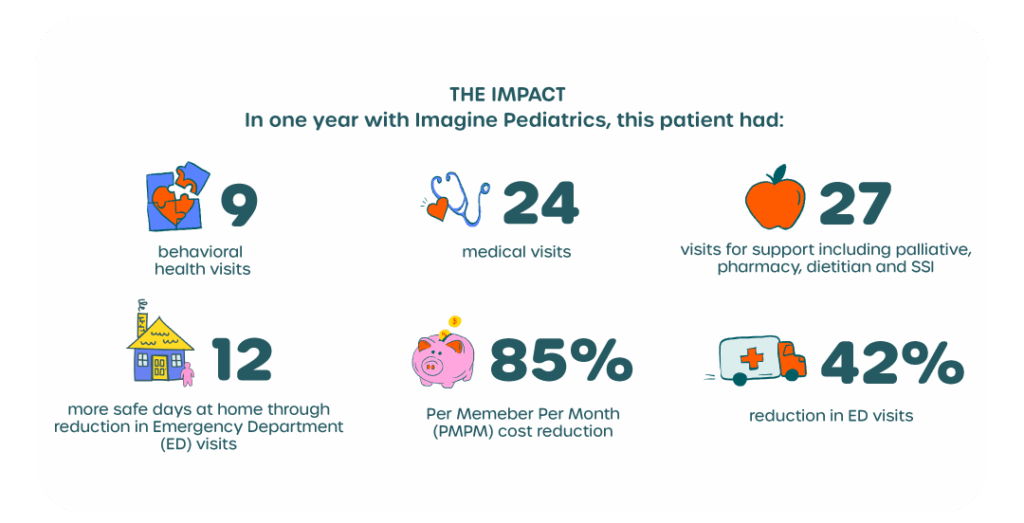
Real-World Impact
In less than three years, the Imagine Pediatrics model is already demonstrating how virtual and in-home pediatric value-based care drives measurable results for children, families, clinicians, and health plans.
For children, the impact is clear: more stability at home and fewer preventable emergencies. More than 5,000 preventable emergency and urgent care visits have been prevented through timely interventions, and 80 percent of those children required no additional acute care in the following month.
For caregivers, the burden of navigating fragmented systems is easing. Families report greater confidence and satisfaction, reflected in a Net Promoter Score of +86, far exceeding the industry average of 20 to 60.
For pediatricians and clinicians, the model reinforces relationship-based care. Continuous, real-time data enables teams to collaborate across disciplines, fill care gaps, and extend the reach of existing providers with 24/7 coverage and consistent follow-up.
For health plans, these results translate into performance and partnership. With Imagine Pediatrics, more than 70,000 children with special health care needs are now served through value-based arrangements that close quality gaps, lower total cost of care, and improve member and provider experience. Working in risk-based partnerships, Imagine Pediatrics aligns outcomes across these quality, cost and member experience measures with plan priorities and stakeholder expectations — from state agencies to employers — proving that integrated, virtual and in-home pediatric care supports both mission and a scalable financial model.
How to Move Forward
Providers, health plans, caregivers, and policymakers each face different challenges, but all share the goal of better outcomes for children with special health care needs. Pediatric value-based models make it possible to solve these problems and create alignment among all stakeholders.
Here are some of the challenges each group faces today—and how models like this can help address them.
PEDIATRIC CARE PROVIDERS
- Challenge: Providers caring for children with special health care needs in a value-based care framework often face overwhelming administrative tasks, limited time and resources to deliver 24/7 support, and the difficulty of coordinating across fragmented systems.
- Solution: Team-based, tech-enabled models can extend care beyond the clinic walls. By integrating medical, behavioral, and social support and sharing real-time data, these models help lighten administrative burden and strengthen continuity, while keeping the trusted provider-family relationship intact.
HEALTH PLANS
- Challenge: Health plans are under constant pressure to improve quality, manage total cost of care, and improve member experience. Yet most pediatric models are not built to meet the complexity of children with special health care needs or to align meaningfully with plan goals.
- Solution: Effective partnerships require continuous collaboration, shared accountability, and data transparency. A strong value-based relationship is anchored in common outcomes across quality, cost, and experience — and supported by deep collaboration, real-time analytics that surface population-level insights. By aligning on outcomes like safe days at home and maintaining open, ongoing communication, plans and care partners can adapt together as needs evolve, ensuring that value-based care truly delivers on its promise.
CAREGIVERS
- Challenge: Families of children with special health care needs often feel isolated, overburdened, and responsible for stitching together fragmented care across multiple systems. Their perspectives are vital to understanding a child’s needs, yet too often they are overlooked or unheard.
- Solution: Multidisciplinary care models that provide 24/7 virtual and in-home access create a genuine partnership with families. Each child is empaneled to a consistent team that delivers both proactive and acute care, centered on family goals and informed by caregiver insight. When caregivers feel heard and supported, they become empowered participants in their child’s care rather than coordinators of disconnected services. This trust builds the foundation for better outcomes, transforming care from episodic and reactive to continuous and responsive. Integrated medical, behavioral, and social support gives families the confidence and practical help they need to keep their children safe, stable, and thriving at home.
POLICYMAKERS
- Challenge: Policy shifts can unintentionally destabilize value-based care efforts, creating churn and uncertainty that undermine continuity. Current funding and quality measures rarely capture what matters most to families.
- Solution: Policy frameworks that support integrated, wraparound care — especially in Medicaid pediatric value-based care — can make integrated care sustainable. Stable funding, interoperability, and pediatric-specific measures will help models that are working today reach more families tomorrow. A better way of caring for children with special health care needs already exists. By aligning providers, plans, caregivers, and policymakers, we can scale the innovation and help families experience more safe days at home.
Conclusion
Personalized pediatric value-based care models make continuity possible, and continuity delivers what families value most: more safe days at home. We’re seeing results that matter and now is the moment to scale what works. Providers can partner with other professionals to extend continuity beyond the clinic, health plans can partner with organizations having shared incentives and supporting innovative metrics like safe days at home, and policymakers can enable interoperability and stable, child-specific measures.
The results are clear, and the model is working. But children with special health care needs cannot wait for incremental change. Providers, health plans, and policymakers must act now to align policy, payment, and care around what matters most to families: integration, personalization, and more safe days at home. The time to act is now. A better approach to pediatric health care is within reach, and we are committed to seizing it today.
# # #
About Imagine Pediatrics
We are an innovative, tech-enabled, pediatrician-led medical group delivering 24/7 virtual and in-home pediatric care to children with special health care needs. Our multidisciplinary team of doctors, nurses, therapists, social workers, pharmacists, and other clinical staff is available any time of the night or day to provide fully integrated medical, behavioral, and social care virtually and in-home.
We provide unlimited access to specialized pediatric clinical programming purpose-built for children with acute and longitudinal medical and behavioral health conditions. Our multidisciplinary team works in partnership with pediatricians, specialists, home health and private duty nursing agencies, durable medical equipment (DME) providers, and community resources to provide our patients and their caregivers with expanded access to integrated medical, behavioral, and social care.
We do not replace a child’s care team or the relationship with their pediatrician. Instead, we team with their existing providers and support patient care with enhanced services through a care collaboration approach. We partner with health plans to serve children with special health care needs via total-cost of-care and quality performance-based risk arrangements that align our economic model with outcomes for our patients and partners.